Notes For All Chapters Biology Class 11 CBSE
Each and every cell of a multicellular organism require food, oxygen and vital components to survive. Simultaneously as a result of metabolism, cell also produces some useful and waste products. Substances that are useful, are transported to other cells, while harmful or waste substances are removed from the body. Thus, it is essential to have efficient mechanisms to move these substances to and from the cells.
To carryout these processes, a carrier inturn is required by the body cells, providing them with essential components (i.e., food, oxygen, etc) and that helps in the distribution of useful products and elimination of waste products. Thus, circulatory system is formed by the carrier, a fluid medium that circulates throughout the body and fulfils the need of the body cells.
Topic 1 Blood and Lymph
Simple organisms such as sponges and coelenterates are single-celled and are in direct contact with atmosphere, thus they do not require any circulatory system for this. They instead circulate water from their surroundings through their body cavities, facilitating the cells to exchange these substances.
In more complex organisms special fluids are used to transport these substances within the body.
Blood and lymph are the two types of fluids that act as a carrier in the body. Blood is a special connective tissue comprising of a fluid matrix, plasma and formed elements. Plasma forms the fluid medium in which the blood cells (corpuscles) float and carryout important functions.
It forms about 30-32% of the total extracellular fluid. Total volume of blood in an adult person is about 5-5.5 L
Plasma
It is a straw coloured, viscous in nature, slightly alkaline aqueous solution. It forms about 55% of the blood.
Composition of Plasma
It is composed of many organic and inorganic substances, which includes 90-92% water and 6-8% solutes in it.
The solutes found in plasma are various ions (likeNa+, Mg2+, Ca2+,HCO3–, etc.), glucose, traces of other
sugars, plasma proteins, amino acids, hormones, cholesterol, other lipids, urea, other wastes and other organic acids.
Factors for clotting or coagulation of blood are also present actively in the plasma. Plasma without the blood clotting factors is called serum.
Plasma Proteins
Proteins found in plasma are the important as they are responsible for providing viscosity to the plasma. The major proteins found in plasma are fibrinogen serum, globulins serum and albumins.
Functions of Plasma
It performs various functions in the blood, these are as follows
(a) Helps in transport and uniform distribution of heat all over the body.
(b) Provides body immunity.
(c) Maintenance of blood pH.
(d) Provides prevention of blood loss.
(e) Fibrinogen help in blood clotting, globulin help in defense mechanism, albumin maintains osmotic balance.
Formed Elements
The formed elements or blood corpuscles includes erythrocytes, leucocytes and platelets.These constitute about 45% of the blood.
1 Erythrocytes (Red Blood Cells)
These are the most abundant of all cells found in the blood. They are red in colour due to the presence of a pigment called haemoglobin, which acts as an oxygen carrier. The formation of RBCs takes place in the red bone marrow in the adults.
Shape, Size and Structure
RBCs are biconcave, disc-shaped cells with the diameter of about 7-8 micron. The shape of RBC is slightly variable. As there are no cell organelles found in it, whole volume is filled with haemoglobin.
Camel and llama are exceptional among mammals in having oval RBCs.
Number
A healthy individual has about 12-16 gms of haemoglobin in every 100 mL of blood.
* In men, the average number of RBC is about 5-5.5 million per cubic millimeter (mm3) of blood.
* In women, the average number is about 4.5-4. mm3 of blood.
Note:
The number of RBCs may vary depending upon the health factors of an individual and altitude where they live.
Person who lives at 18,000 feet may have as many as (8.3 x 106 RBC/pL). If a fall in number of RBC occurs, the condition is called anaemia whereas, the increase in number is called polycythemia.
Lifespan of RBC
Total lifespan of RBC is 120 days. After which RBC becomes non-functional and gets destroyed.
Disintegration of RBC
The process of disintegration of RBC occurs in liver. The Kupffer’s cells of liver helps in complete disintegration process. The haemoglobin is disintegrated to release iron. Free iron is transported back to the bone marrow and the debris that remains, forms two toxic pigments, i.e., bilirubin and biliverdin (as studied in chapter 16). The remaining membrane of RBC known as ghost (i.e., without haemoglobin) is transported to spleen, where it gets destroyed completely. Due to this reason, spleen is called graveyard of RBC.
2. Leucocytes (White Blood Cells)
These are known to be the most active and motile constituent of blood as well as lymph. They do not possess the red colour pigment (haemoglobin) in them, so, they are colourless in nature.
They are nucleated and are generally short lived. The number of WBCs are relatively lesser in number, about 6000-8000 mm3 of blood.
White blood cells or leucocytes are categorised into two main categories. Such as
i. Granulocytes
They contain granules and have regularly lobed nucleus in the cytoplasm.
The granulocytes are further sub-divided into three main types
(a) Neutrophils These are the most abundant cells (about 60-65%) of the total WBCs. They stain equally well with acidic as well as basic dyes, because they are neutral in nature. These are phagocytic cells that destroy foreign organisms entering the body.
(b) Eosinophils They are characterised by their bilobed nucleus. They are stained bright red in colour with acidic dye (due to the presence of numerous coarse granules in it) such as eosin. They are about 2-3% of total WBCs. They resist infections and are also associated with all allergic reactions. They also help in dissolving blood clot. They help to destroy the toxic substances present in the body.
During allergic conditions, the number of eosinophils increases in the body.
(c) Basophils They contain fewer coarse granules than the eosinophils and can be staioed with basic dyes such as, methylene blue. They are found least abundandy (0.8-1.0%) among WBCs. They secretes histamine, serotonin, heparin, etc., and are involved in inflammatory reactions.
Agranulocytes
They lack granules and have non-lobed, rounded or oval nucleus.
Agranulocytes are also further sub-divided into of two main types
(a) Lymphocytes These are smaller in size and have rounded nucleus. Lymphocytes are of further two types, i.e., B-cells and T-cells. Both of these (i.e., B and T-cells) are responsible for immune responses of the body.
(b) Monocytes These are largest of all types of WBCs but are fewer in number. Mature monocytes are known as macrophages. They helps to kill foreign particles.
Blood Platelets (Thrombocytes)
These are cell fragments produced from megakaryocytes (i.e., the special cells found in the bone marrow).
Structure
These are oval-shaped, disc-like cells found only in mammalian blood. These are devoid of nuclei.
Platelets contain mitochondria, Golgi bodies and some other structures such as granules, tubules, filaments of aetin and myosin, ADP, etc.
Number
Blood normally contains 1,50,000-3,50,000 platelets per cubic meter (mm3). A reduction in their number can lead to clotting disorders which will lead to excessive blood loss from the body.
Life Span
The life span of platelets is only about 7-12 days.
The formation of thrombocytes is called thrombopoiesis.
Function of Blood Platelets
Their main function in the body is to release a variety of substances, most of which are involved in coagulation or clotting of blood.
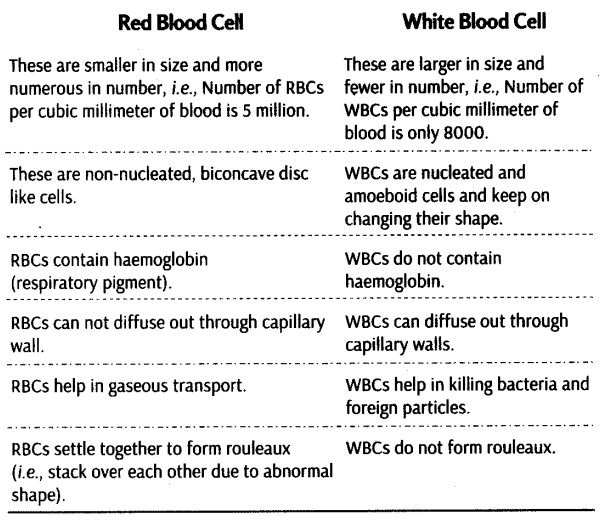
Differences between Red Blood Cells and White Blood Cells
Blood Groups
Although blood of every human being appears to be similar in appearance but, it differ in certain aspects. The plasma membrane of RBCs contain certain glycoproteinaceous molecules known as antigens, which differ in different persons. Thus, providing them different blood groups.
Two important common types of blood grouping found in human beings are called universal donors. Whereas, the persons with blood AB can accept blood from any blood group (i.e., AB as well as A, B, and O). Hence, are called universal recipients.
1. ABO Grouping
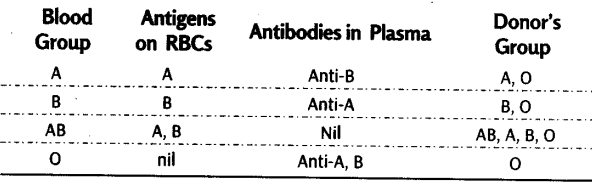
It was reported by Karl Landsteiner that ABO blood grouping is based on the-presence or absence of antigen A or antigen B on the surface of RBCs (chemicals that can induce immune response). Similarly the plasma of different individuals contain two natural antibodies (which are proteins produced in response to antigens).
A, B and 0 blood groups were discovered by Landsteiner (1900). Blood group AB was discovered by de Castello and Steini (1902).
People with blood group A have the antigen A on the surface of their RBCs and have antibodies against antigen B in their plasma. While in the people having blood group B, the case is just vice-versa to blood group.
Apart from both these blood groups (i.e., A and B) people with blood group AB have both antigen A and B on their RBCs surface and no antibodies for either of the antigens in their plasma.
In people with blood group O, both antigen A and B are not present on their RBCs but they have antibodies against the plasma. This distribution of antigens and antibodies in the four blood groups (A, B, AB and O).
These can be well explained through the table given below
2. Rh Grouping
Apart from the antigens discussed in the previous section, another antigen, known as Rh antigen (similar to the one present in Rhesus monkey) is also found on the RBCs surface in majority of humans (nearly about 80%). Individuals having Rh antigen are called Rh positive (Rh+) and those without the Rh antigen are called Rh negative (Rh–).
Rh group is mandatory to be matched before transfusion of blood. An Rh– person if gets exposed to Rh+ blood, will form specific antibodies against the Rh antigens.
Rh Incompatibility During Pregnancy
A special case of mismatching of Rh group or Rh incompatibility has been observed between the Rh– blood of a pregnant mother with Rh+ blood of the foetus (born out of a marriage between Rh- woman and a Rh+ man).
In such a case, mother becomes sensitive, while carrying a Rh+ baby in her womb. The reason is that some of the RBCs from the developing foetus enters into the blood stream of the mother during development. This causes the development of anti-Rh antibodies.
The Rh antigens of the foetus do not get exposed to the Rh– blood of the mother in case of first pregnancy (because two blood remain separated by placenta).
However, during delivery of the first child, there occurs a possibility that maternal blood may get exposed to small amounts of Rh+ blood from the foetus.
Hence, preparing antibodies against Rh antigens in her blood.
Thus, in case of her subsequent pregnancies, Rh+ foetuses get exposed to the anti-Rh antibodies. These will leak into the blood of the foetus (Rh+) and destroy foetal RBCs.
This could be fatal to the foetus or could cause severe anaemia and jaundice to the body. This is known as erythroblastosis foetalis.
In humans, during transfusion of blood, the blood of a donor has to be carefully matched to the blood of a recipient before transfusing, so as to avoid the problem of clumping (destruction of RBC).
A person with blood group O can donate blood to persons with any of the other blood group (i.e., either A, B, AB and O). Hence, are
This condition can be avoided by administering anti-Rh antibodies to the mother immediately after the delivery of the first child.
Rh factor was discovered by Landsteiner and Weiner (1940) after immunising the rabbits with the blood of a monkey (Macaca rhesus).
There are 30 or so known antigens on the surface of red blood cells that give rise to different blood groups, e.g., MN, etc.
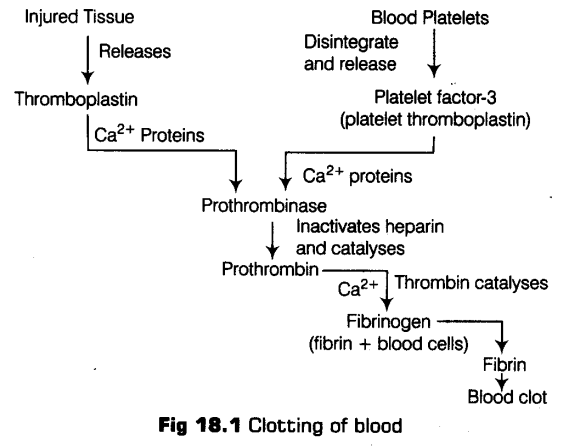
Coagulation of Blood or Clotting of Blood
When an injury is caused, the wound does not continue to bleed for a long time and the blood usually stops flowing after sometime. It is the natuial property exhibited by the blood to check the excessive loss of blood from an injury or trauma. Clotting of blood is a complex process that involves various steps for its completion.
Natural Anticoagulants
Normally, inside an intact blood vessel, the blood does not coagulate because of the presence of an active anticoagulants, i.e., heparin or antiprothrombins. Apart from this procoagulants are also present in the blood but in their inactive forms.
Haemophilia is a genetic disease, which is caused due to deficiency of prothrombin, fibrinogen and vitamin-K. In this condition, the blood does not clot if there is any injury.
Formation of a Clot
An injury or trauma causes, stimulation of platelets in the blood to release certain platelet factors which inturn activates the mechanism of coagulation or clotting. Thromboplastin, a lipoprotein helps in clot formation.
It occurs in following three steps
(i) Thromboplastin, helps in formation of an enzyme prothrombinase (which inactivates heparin) that converts the inactive plasma protein, i.e., prothrombin into its active form thrombin.
(ii) Thrombin thus, acts as a proteolytic enzyme to convert fibrinogen molecule (produced from the liver in the presence of vitamin-K) to form insoluble fibrin monomer.
This reaction required thrombokinase an enzyme complex, which is formed by a series of linked enzymatic reactions (cascade process) which involves a number of various factors present in the plasma in their inactive state.
Both the changes mentioned above requires Ca2+ ions for their reaction.
(iii) These fibrin monomers polymerise to long, sticky fibres. The fibrin threads forms a fine network of threads called fibrins, in which dead and damaged formed elements of blood are trapped.
This finally leads to the formation of a clot or coagulum, which is a dark reddish brown scum formed over the surface of injury.
Certain factors released by tissues also help in initiating coagulation at the time of injury.
Functions of Blood
Blood performs the following important Junctions
(i) Helps in transportation of respiratory gases (i.e., O2, CO2, etc).
(ii) Helps in healing of wounds.
(iii) Maintains body pH, water and ionic balance. .
(iv) Fight against infections by forming body immunity.
(v) Also helps in transportation of hormones from endocrine glands to target organs.
(vi) Coagulation of blood.
(vii) Helps in transportation of body wastes from different body parts to kidneys.
(viii) Maintains normal body temperature.
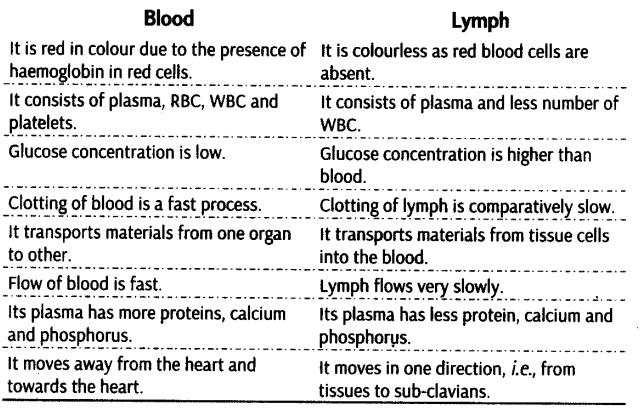
Lymph (Tissue Fluid)
It is another fluid connective tissue that floats inside specialised vessels known as lymph vessels.
Composition
It is a colourless fluid containing high concentration of WBCs (specialised lymphocytes). The overall composition of lymph is similar to blood with the exception of absence of RBCs, platelets and some plasma proteins and in having less Ca and P than blood. It also contains all the ions, present in the blood plasma.
Lymphatic System
It is an elaborate network of vessels, which collects the interstitial fluid (tissue fluid), along with some protein molecules drains it back into the major veins. The lymphatic vessels are present in all tissues (except the central nervous system and cornea).
Formation of Lymph
As the blood passes through the capillaries of the arterial system into the tissues, some water along with many water soluble substances come out in the spaces between the cells of tissues.
But a very small amount of proteins come out from the capillary with the plasma (leaving the larger proteins and most of the formed elements in the blood vessel).
The fluid thus, released out is called interstitial fluid (tissue fluid) or Extra Cellular Fluid (ECF).
After entering the lymph vessel, the ECF becomes lymph.
Functions of Lymph
Lymph performes the following important functions
(i) It acts as an important carrier of nutrients, hormones, etc.
(ii) Absorption of fat also occurs through lymph in the lacteals present in the intestinal villi.
(iii) Also helps in the renewal of ECF.
(iv) Maturation of lymphocytes, i.e., B-cells and T-cells occur with the help of lymph nodes, releasing them into the lymph.
(v) Helps in keeping tissue cells moist.
The lymph first reaches the lymph nodes like thymus, tonsils, Payer’s patches, spleen, etc., in the body.
Differences between Blood and Lymph
Topic 2 Circulatory Pathways
It is already clear by the previous topic that blood and lymph are the important fluids in the body that acts as a carrier in transporting nutrients, hormones, etc.
Now, the question arises what makes this blood to circulate. So, the answer to this question lies in the fact that to circulate this blood throughout the body, a pump is required known as heart.
Depending upon the circulatory patterns in higher organisms the circulatory system are offollowing two types
1. Open Circulatory System
It is the type of circulatory system in which blood pumped by the heart is passed through a vessel into the spaces or body cavities known as sinuses. From there the blood is collected by large veins, which opens into the heart.
In this type of system, the blood does not contain the respiratory pigment and if present, is dissolved in plasma.
This type of system is found in arthropods and molluscs.
There is no capillary system (i.e, interconnecting vessels) found in this type (i.e, open type) of circulatory system.
2 Closed Circulatory System
In this type of circulatory system, the blood pumped by the heart is always circulated inside the vessels {i.e., it is never present in large spaces or sinuses).From evolutionary point of view, this pattern is considered to be most advantageous as it supplies blood to the deepest tissues of the body. It is found in annelids and chordates.
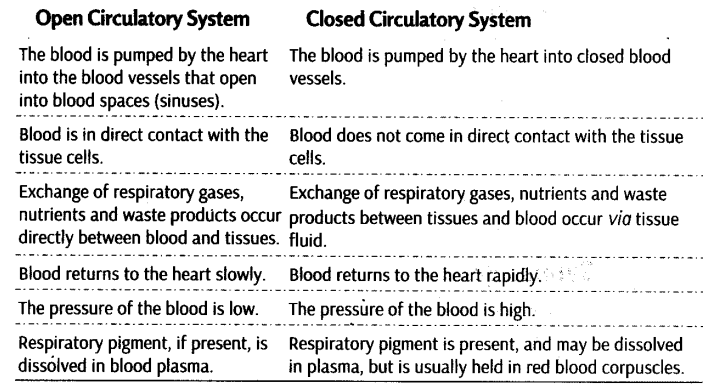
Differences between Open and Closed Circulatory System
Heart (The Pumping Organ in Vertebrates)
All vertebrates possess a muscular chambered heart.
Depending upon the different types of circulation in them heart is of following three types
1. Two-Chambered Heart
This is found in fishes mostly. It comprises of an atrium and a ventricle. During circulation of blood, the heart pumps out deoxygenated blood. This blood gets oxygenated by the gills and is then supplied to the body parts from where the deoxygenated blood is returned to the heart. Hence, the type of circulation is called single circulation.
2 Three-Chambered Heart
Amphibians and reptiles (except crocodiles) have a three-chambered heart. This type of heart comprises of two atria and a single ventricle.
During the circulation of blood, the left atrium receives the oxygenated blood from the gills/lungs/skin and the right atrium receives the deoxygenated blood from the other body parts. The blood gets mixed up in the single ventricle which further pumps out the mixed blood. This type of circulation- is called incomplete double circulation.
3 F0lir-Chamb6r6d Heart
Crocodiles, birds and mammals possess this type of heart. It comprises of two atria and two ventricles. During the course of circulation, the oxygenated and deoxygenated blood is received by the left and the right atria respectively.
The blood from each atria are passed onto the ventricles of the same sides (i.e., left and right ventricles). Unlike, three-chambered heart, in which the bipod through the ventricles {i.e., four-chambered) is pumped out without any mixing {i.e., two separate circulatory pathways are present in these organisms). Hence, this type of circulation is called double circulation.
Human Circulatory System
Circulatory system in humans is also known as blood vascular system. It consists of a muscular chambered heart, a network of closed branching blood vessels and the fluid that is circulated, i.e., blood.
Position and Appearance
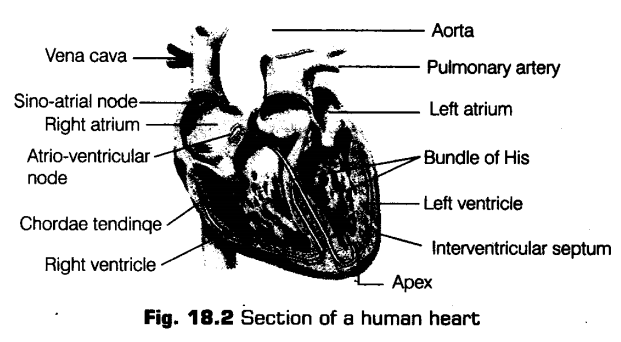
Heart is a mesodermally derived organ, situated in the thoracic cavity in between the two lungs. It appears to be slightly tilted towards the left side. It is a hollow, fibromuscular organ, slightly conical in shape of about 12 cm length and 9 cm breadth. The upper broad part is called the base and the lower narrow part known as the apex. It has a size of a clenched first.
Protective Covering
The heart is protected by a double walled membranous sac or a bag called pericardium, enclosing pericardial fluid. This pericardial fluid helps in keeping the surface of the heart moist, so as to protect it from shock and mechanical injuries and also allows its free movements.
Structure of human heart can be studied under two heads for easy understanding, i.e., external and internal structure. ‘
External Structure
Externally, the human heart is composed of four chambers, i.e., two relatively small upper chambers called auricles (sing, atria) and two larger lower chambers called ventricles.
The right atrium is slightly larger than the left atrium. Both these atria are meant to receive blood from different body parts.
Internal Structure
Internally, the chambers of heart, i.e., two auricles (atria) and ventricles are separated by different septa and valves.
Auricles (Atria)
These are the upper two thin-walled and smaller chambers. These serve to receive the blood, therefore are called receiving chambers (right atrium and left atrium). Both the right and the left atria are separated by a thin, muscular wall known as interatrial septum.
(AS) Right Atrium This right chamber deals with only impure (deoxygenated) blood. It receives impure blood from various parts the body, through two major veins, i.e., superior and inferior vena cana. It also receives blood from the walls of the heart itself (through a coronary sinus).
(b) Left Atrium This chamber is meant to deal with only pure (oxygenated) blood. It receives blood (pure) from lungs through two pulmonary veins (i.e., one from the each lung).
Ventricles
These are lower two chambers of the heart, that pumps the blood away from the heart. Thus, function as pumping chambers. Both the right and the left ventricles are separated by the interventricular septum. The atrium and the ventricle of the same side are also separated by another septum, a thick fibrous tissue called atrio-ventricular septum (i.e., AY septum).
As ventricles major function is pumping of blood, due to this, they need thick muscular walls.
(a) Right Ventricle It receives impure blood from right atrium and pumps to pulmonary artery, which further takes this blood to lungs for purification.
(b) Left Ventricle It receives pure (oxygenated) blood from left atrium and pumps its pure blood to aorta (largest artery in the pathway), which inturn takes this blood to whole body and organs.
Cardiac Valves
Apart from septum, heart is also separated by the various valves. These valves acts as a door like structure in the heart that serves to maintain the unidirectional flow of blood.
Different valves present in the heart are given below
(i) Tricuspid Valve It is formed by three muscular flaps or cusps to guard the opening between the right atrium and the right ventricle.
(ii) Bicuspid Valve (Mitral valve) It is the type of valve that guards the opening between the left atrium and the left ventricle.
(iii) Semilunar Valve The opening of the right and the left ventricles into the pulmonary artery and the aorta respectively are provided with the semilunar valves.
Functions of Cardiac Valves
The valves in the heart allows the flow of blood only in one direction, i.e., from the atria to ventricles and from the ventricles to the pulmonary artery or aorta but also prevent any backward flow of blood.
Conducting System of Heart
The entire heart is made up of cardiac muscles. The ventricular walls are thicker than that of the atrial walls. The rhythm of heart is maintained by a highly specialised cardiac musculature called the nodal tissue distributed in the heart.
1. The Sino-Atrial Node or SA Node (SAN)
SA node is a small flattened patch of tissue present in the right upper corner of the right atrium. The impulse generated by this node spreads in all directions of the heart (i.e., go to both auricles and causes their relaxation and contraction).
2. The Atrio-Ventricular Node or AV Node (AVN)
The signals becomes weak when they reach ventricles because ventricles are far away from SA node thus, to strengthen these signals, another mass of tissue is seen in the lower left corner of the right atrium close to the atrio-ventricular septum {i.e., at the junction of ventricles and atrium) known as AV node. This is also known as pacesetter.
AV node is used to receive the impulses from the SA node through an internodal pathway.
3 Bundle of His
A bundle of nodal fibres, i.e., atrioventricular bundle (AV bundle) continues from the AV node, which passes through the atrio-ventricular septa to emerge y on the top of the inter-ventricular septum immediately dividing into a right and left buqdle.
This bundle give rise to a network of minute fibres (which are myocardial in origin) throughout the ventricular musculature of the respective side known as Purkinje fibres. These fibres along with the right and left bundles are called bundle of his.
It generates impulses for beating. Normally it does not generates impulse,but strengthen them.
The Purkinje fibres supply impulses to all portions of ventricular walls.
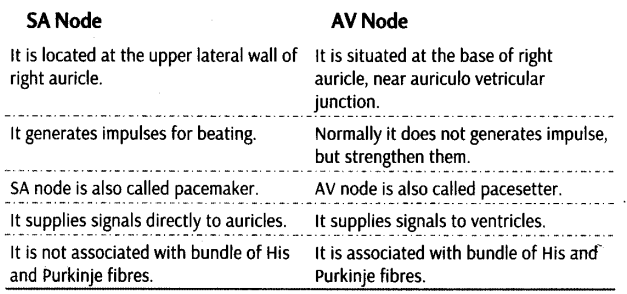
Differences between SA Node and AV Node
Working of Nodal Tissue
The nodal musculature possess the ability of generating action potentials without any external stimuli, i.e., it is autoexcitable. However, the nodal system generates different number of action potential at different parts in a minute. The SAN can generate the maximum number of action potentials, i.e., 70-75 min .
It is also responsible for the initiation and maintenance of the rhythmic contractile activity of the heart. Therefore, the SAN (i.e., SA node) is also called pacemaker.
Our heart normally beats 70-75 times in a minute [i.e., average 72 beats/min).
Blood Vessels
As man has a closed circulatory system the blood strictly flows in a fixed route through arteries and veins maintain a continuous flow throughout the body inside the closed tubes or blood vessels.
These tubes or vessels are of mainly two types
Arteries
These blood vessels carry blood from the heart to different body parts. All arteries carry pure or oxygenated blood, with the exception of pulmonary artery that carries the impure or deoxygenated blood {i.e., from heart to the lungs for purification). As the walls of arteries are thick and non-collapsible, the pressure inside them is very high.
Arteries are much deeply placed in the body.
Features of Arteries
(а) Valves are absent in arteries.
(b) Arteries are divided into five branches, known as arterioles, which are further divided to form finer branches, called capillaries.
Veins
These are another type of blood vessels that bring blood from different body parts to the heart, i.e., carry blood towards the heart. All veins are meant to carry impure blood except the pulmonary vein that carries pure blood, i.e., from lung to the heart. Veins are provided with valves to prevent backward flow of blood.
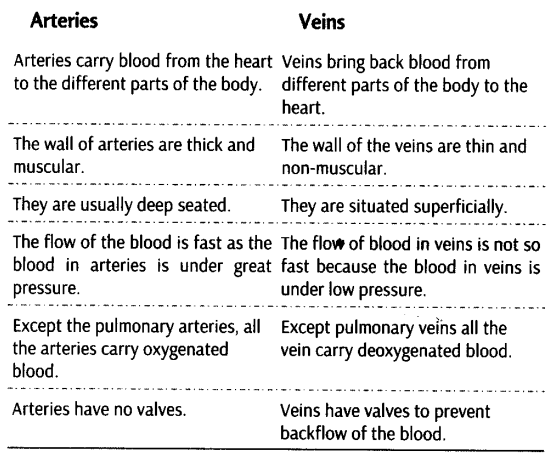
Differences between Arteries and Veins
Cardiac Cycle
The heart pumps the blood to all parts of the body. The changes that takes place in heart during one heart beat, together constitutes cardiac cycle.
The heart beats at an average rate of about 72 times/min. Thus, the total duration of a cardiac cycle is 0.8 s. During a heart beat, the contraction and relaxation of atria and ventricles takes place.
The phase of contraction is known as systole, while the relaxation phase is called the diastole. Thus, a single heart beat consists of a systole and diastole of both the atria and the ventricles.
To begin with the cardiac cycle, all four chambers of heart are in a relaxed state, i.e., they are in joint diastole, during which, the blood flows from the superior and the inferior venae cavae into the atria and from there to the respective ventricles through auriculo-ventricular valves.
The complete cardiac cycle is comprised of following events that takes place in a sequential manner
Atrial Systole
A wave of contraction occurs from anterior to posterior side stimulated by the SA node. The blood flows from the pulmonary veins and vena cava into the left and right ventricles respectively as the tricuspid and bicuspid valves are open.
During this time the blood does not return to the great veins (as blood is already present in them). The semilunar valves are closed. The atrial systole increases the flow of blood into the ventricles by about 30% (as 70% filling of ventricles occurs passively during relaxation of ventricles, before the atrial contraction).
At the end of the atrial systole, there start relaxation of the atria (atrial diastole) and contraction of the ventricles (ventricular systole) simultaneously.
The atrial systole occurs for 0.1s, while the atrial diastole on the other hand is of about 0.7s.
Ventricular Systole
This step involves the simultaneous relaxation of atria (atrial diastole) and contraction of ventricles (ventricular systole).
As the contraction of the ventricles begins, the pressure of blood rises in them almost immediately (above the pressure in the atria). This rapidly closes the atrio-ventricular valves, in order to prevent the back flow of blood from ventricles to atria.
The conduction of action potential to the ventricular side occurs by the AV node and AV bundle from where the bundle of His transmits it through the entire ventricular musculature.
The contraction of ventricles thereby, increases the ventricular pressure causing the closure of the tricuspid and bicuspid valves due to attempted backflow of blood into the atria.
Finally, due to this, the increase in the pressure occurs in the great arteries (i.e., pulmonary and aortic arches), so, semilunar valves guarding the pulmonary artery (right side) and the aorta (left side) are forced open and blood enter through great arteries into ventricles.
When ventricles relax (ventricular diastole), the ventricular pressure falls which causes the closure of semilunar valves preventing the backflow of blood into the ventricles.
A further decline in the ventricular pressure, pushes open the tricuspid and bicuspid valves by the pressure in the atria exerted by the blood, which was being emptied into them by the veins. This allows the blood to move freely to the ventricles once again.
The ventricles and atria are now again in a relaxed state (joint diastole) as earlier.
Soon, the SAN generates a new action potential and the events described above sequencially repeated to continue the process (next cardiac cycle).
Heart Rate and Cardfac Output
We have just studied that, our heart beats for about 72 times per minute (on an average). This concludes that in a single minute, many cardiac cycles are performed. Thus, deducing that duration of a each cardiac cycle is 0.8 s.
During each cardiac cycle (i.e. in one beat) each ventricle pumps out about 70 mL of blood known as stroke volume.
The volume of blood pumped out by each ventricle in one minute is called cardiac output.
We know that, in one minute heart beats for 72 times. Thus, cardiac output will be 5000 mL or approx. 5L in a normal individual.
Thus, Cardiac output = Stroke volume x Numbers of beats /min.
It is to be noted that the body has the ability to alter stroke volume as well as the heart rate and thereby, the cardiac output.
For example Athlete has much higher cardiac output than the normal man.
Heart Sounds
During each cardiac cycle, two prominent sounds are produced which can be easily heard by a stethoscope (an instrument used for the amplification of sound). This allows to hear sounds and pulse of an individual. The basic reason for the production of these sounds is the closure of various valves.
The sounds cardiac produced during each heart beat are as follows
i. Lub It is the first sound, being produced when inter auriculoventricular valves (tricuspid and bicuspid valve) are closed. This.marks the end of the atrial systole and beginning of ventricular systole.
ii. Dub It is the $ pond sound being produced when semilunar valves (of aorta and pulmonary artery) get closed. This marks the end of ventricular systole.
Electrocardiograph EGG:
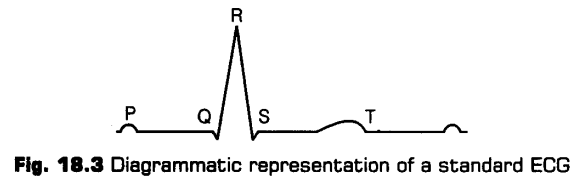
It is a graphical representation of the electrical activity of the heart during a single cardiac cycle. The electrocardiogram is obtained by a machine known as electrocardiograph. The study or the process of recording of electrocardiogram is called electrocardiography.
Einthoven (1903) is known as ‘father of electrocardiography’. The impulse generated by the SA node causes contraction and relaxation of heart chambers.To obtain an ECG, a patient is connected to the machine with three electrical leads (i.e„ one to each wrist and one to the left ankle), monitoring the activity of heart continuously and heart’s functioning is evaluated by attaching multiple leads to the chest region.
Reading an ECG
An ECG consists of five peak, identified with the letter P to T that corresponds to a specific electrical conductivity of the heart.
These corresponds to a specific electrical activity of the heart as follows
i. P Wave It is the first and the foremost wave of low amplitude. It represents the electrical excitation or depolarisation of the atria which, leads to contraction of both the atria.
ii. QRS Wave or Complex The Q, R and S wave together forms the QRS complex. This represents the depolarisation of the ventricles, which initiates the ventricular contraction.
It marks the spread of impulse from AV node to ventricles, through bundle of His and Purkinje fibres. The contraction starts shortly after Q and marks the beginning of the systole. R is the most conspicious wave out of all, having highest amplitude.
iii. T Wave It is a broad and smoothly rounded deflection, which represents the return of the ventricles from excited to normal state (repolarisation). The end of T wave marks the end of systole. It has been observed that, by counting the number of QRS complexes, that occur in a given time period, one can easily determine the rate of heart beat of an individual.
However, the deviation in the EGG of any person from the normal shape ECG, indicates a possible abnormality or a diseases. .
Significance of ECG
ECG is proved to be of great clinical significance due to following reasons
(a) It gives accurate information about the normal functioning of atria and ventricles.
(b) Indicates the functioning of valves.
(c) ,$lso helps in indicating any damage to local tissues of the heart in detection of over growth of cardiac/heart chambers.
Tachycardia is a term applied to a rapid heart or pulse rate (over 100/min). Bradycardia is the term indicating a slow heart or pulse rate (under 50/min).
Leave a Reply